Press Releases & Statements
Nippon Steel Deal — Allegheny Conference CEO Stefani Pashman
May 23, 2025Press Releases & Statements
Pittsburgh Region Celebrates Hitachi Energy’s Expansion Plans
April 11, 2025Press Releases & Statements
Pittsburgh Region Sparks Key Energy Opportunity with New Power Generation Facility
April 9, 2025Press Releases & Statements
Pittsburgh Region Welcomes Country’s Largest Natural Gas-Powered Data Center Campus
April 3, 2025News
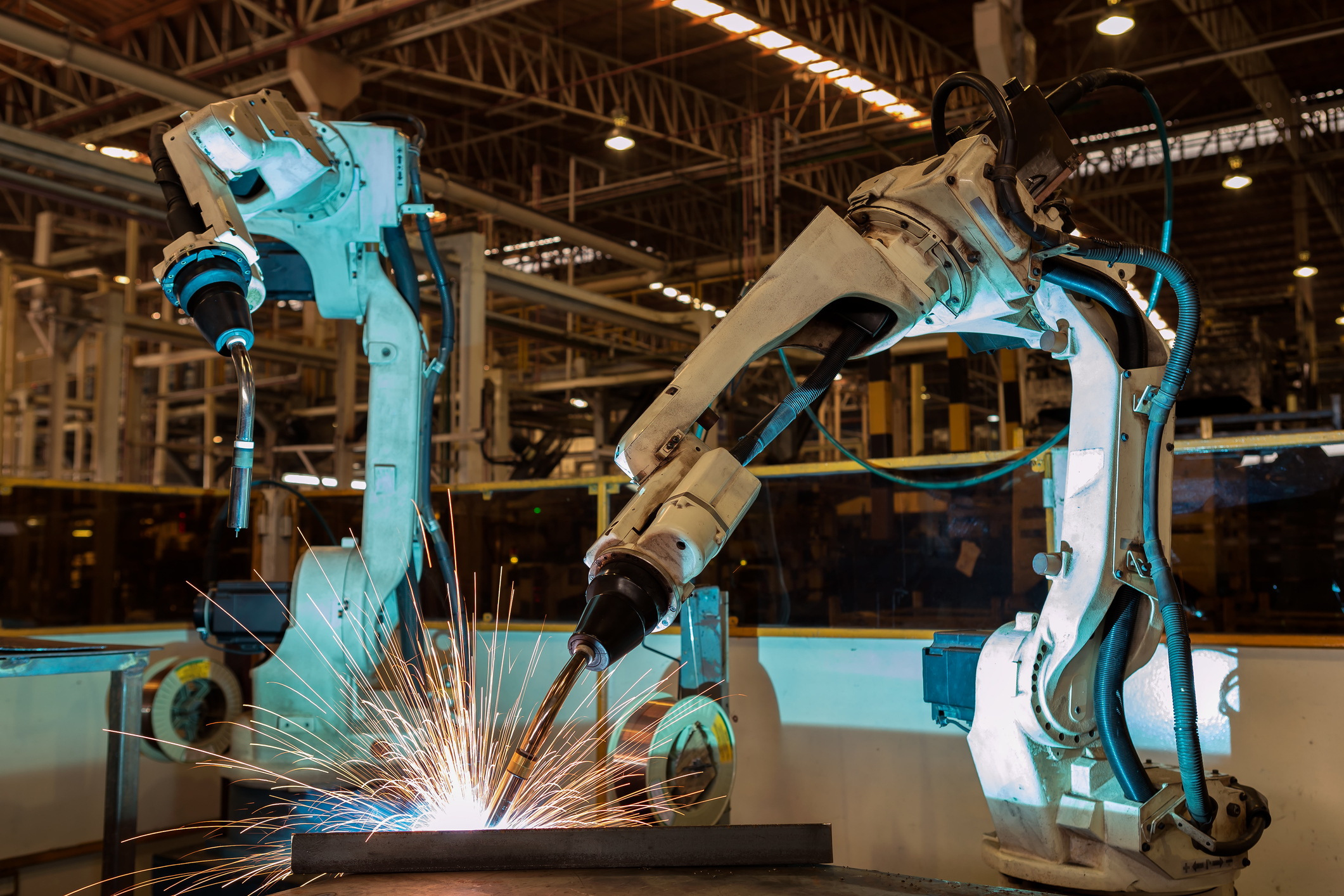
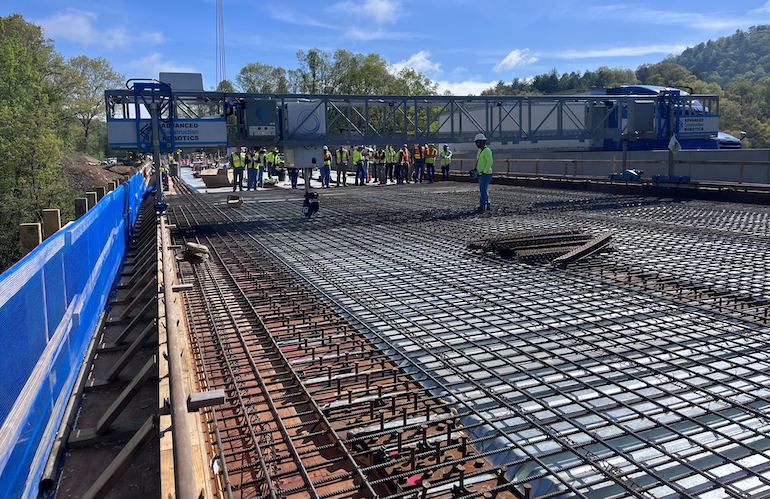
Robots greet students, sales force at third annual Robotics Discovery Day in Pittsburgh
November 20, 2024News
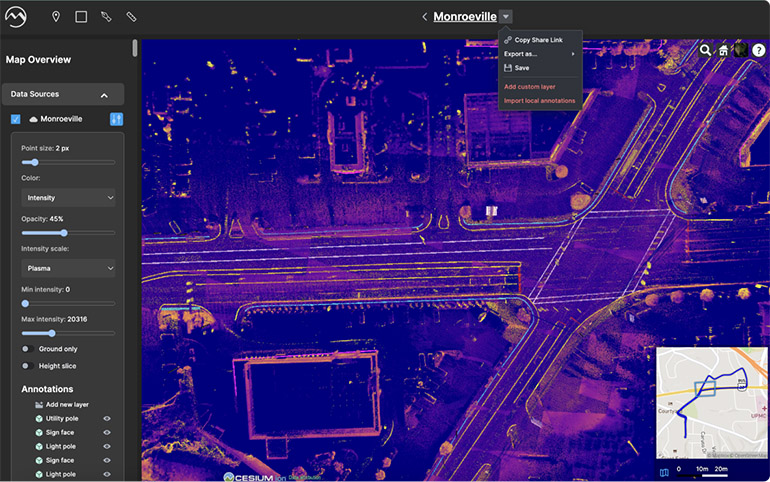
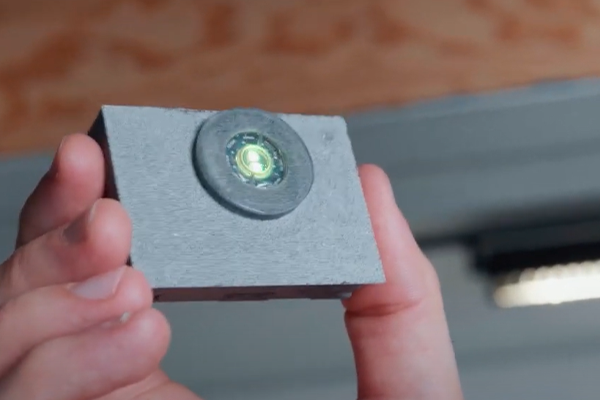
Mach9 Robotics accelerates geospatial data processing for infrastructure industry
September 16, 2024Press Releases & Statements
Nextracker and JENNMAR Subsidiary JM Steel Bolster U.S. Supply Chain with New Facility Expansion to Triple Capacity for Solar Energy Projects
April 26, 2024Press Releases & Statements
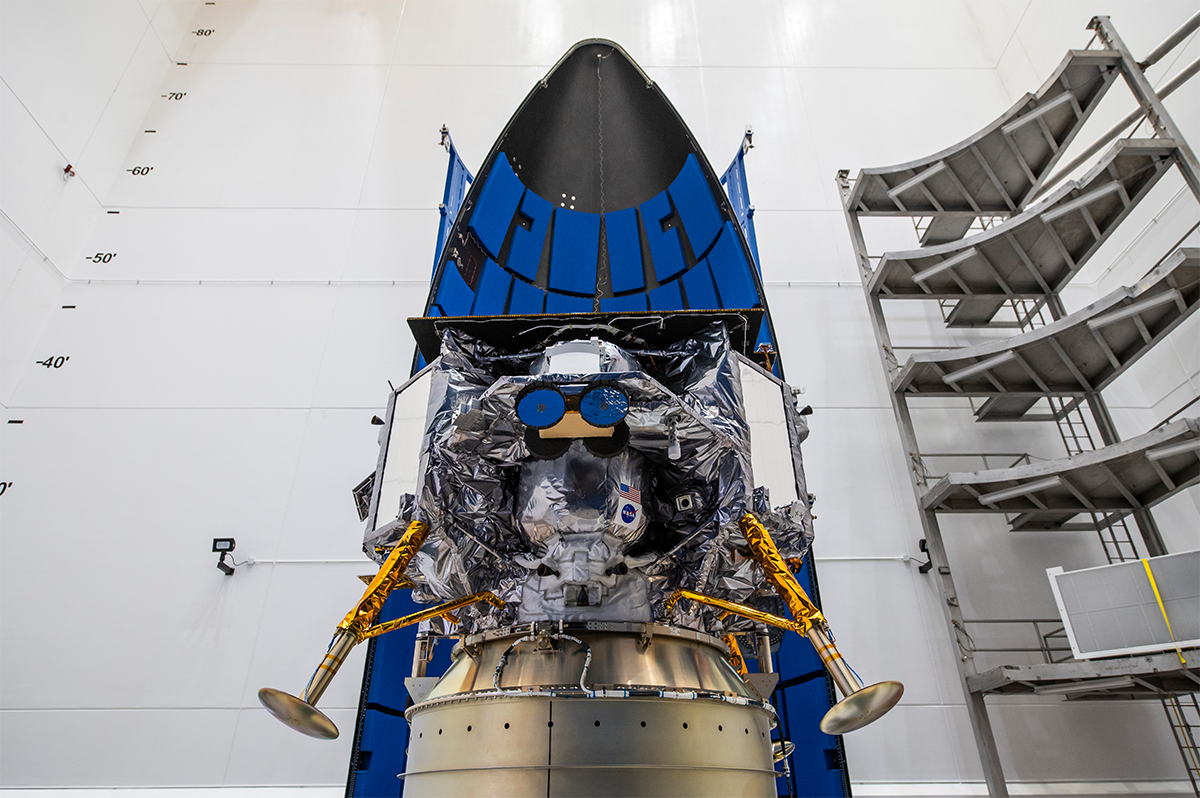
The Pittsburgh Region Will Be on the Global Stage with Its Premiere at CES 2024
January 4, 2024Video
The Great Allegheny Passage - A 150-Mile Trail Connecting Pittsburgh to Maryland
November 30, 2023Video
Bringing Pittsburgh to the World: Pittsburgh Regional Alliance Travel Recap 2023
September 22, 2023News
SoftBank backs new autonomous trucking startup from founders of defunct Argo AI
September 7, 2023News